A systematic review of 33 randomized controlled trials. Of the 27 patients with dvt, 3 had a proximal dvt and 24 had a distal dvt.
(pe) and deep vein thrombosis (dvt) by about 10 events per 1,000 patients treated;
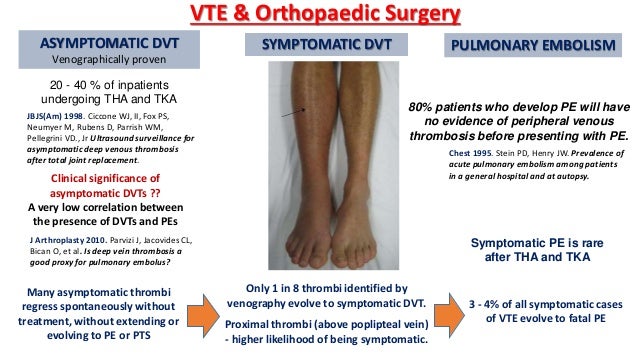
Dvt prophylaxis after surgery. They also noted that postoperative immobilization (p=0.053), hindfoot surgery (p=0.02), increased tourniquet time (p=0.03), and advancing age (p=0.051) were associated with risk of dvt. The incidence of dvt after hip and knee surgery can be more than 60%, with up to 13% subsequently having pulmonary emboli. These authors also concluded that the rate and progression of dvt after foot and ankle surgery is low and does not require routine prophylaxis, even in high risk patients.
Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated. < 0.2 increase by 25 % 4 hours after 4th dose 0.2 to 0.5 no change repeat in 1 week, then monthly thereafter 0.6 to 1 decrease by 20 % 4 hours after 4th dose prevention of dvt/pe 0.2 to 0.5 units/ml > 1 hold for 3 hours, then decrease next dose by 30% 4 hours after 4th dose umhs enoxaparin dosing guidelines ideal body weight Other studies supported that lmwh is better for dvt prophylaxis in tkr compared with warfarin or aspirin.
Review patient status daily (0,2) heparin 5000 units sc q8h (give first dose 2 hrs. Two trials associating longer duration lmwh with reduced risk of vte provided the basis for this recommendation. Use mechanical prophylaxis until contraindication no longer present.
Prophylaxis given (ie, wound haematoma, gastric bleeding, etc) or failure of prophylaxis (ie, proven dvt/pe) within 3 months of surgery. (pe) and deep vein thrombosis (dvt) by about 10 events per 1,000 patients treated; Vte risk is based on the type of surgery and underlying patient�s risk factors.
However, their incidence has increased as awareness has increased. However, the american college of chest physicians(accp) [2] in 2001 published a comprehensive systematic review and guideline on dvt prophylaxis in other specialties. Vte is highest soon after surgery:
Dvt may progress to thrombophlebitis or pulmonary embolism (pe) with increased morbidity and mortality. Patients who develop upper extremity dvts often have multiple comorbidities. A systematic review of 33 randomized controlled trials.
In november 2015, the fda approved dabigatran for prophylaxis of dvt and pe after hip replacement surgery. Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in inpatients undergoing surgery. Historically, upper extremity deep venous thromboses (dvts) have been rare;
The rate of bleeding complications after pharmacologic deep venous thrombosis prophylaxis: Prophylaxis in foot and ankle surgery. Venous thromboembolism (vte) prophylaxis is indicated while in the hospital after major surgery.
Position statement there is currently insufficient data for the american orthopaedic foot & ankle society (aofas) to recommend for or against routine venous thromboembolic disease (vted) prophylaxis for patients undergoing foot and ankle surgery. Further research in this field is both necessary and encouraged. Upper extremity deep venous thrombosis prophylaxis after elective upper extremity surgery.
For hip fracture patients in whom surgery may be delayed, commencing the thromboprophylaxis shortly after admission is suggested. 21,22 in one trial, 28 days were compared to the standard seven days of. After careful review, the sages guidelines committee has approved the.
Major surgeries are categorized as moderate to high risk for vte and need dvt prophylaxis. 49,50 handoll et al 51 reported that lmwh and ufh are similarly effective in preventing dvt after hip fracture surgery, while mismetti et al 52 concluded that vkas are less effective than lmwh, without any significant difference in bleeding risk in patients undergoing. Risk assessment followed by appropriate mechanical or pharmacological prophylaxis will substantially reduce the considerable mortality and morbidity related.
Of these patients, 27 (23.47%) with a surgically treated achilles tendon rupture developed a symptomatic dvt either while waiting for, or after, surgical intervention, with approximately one third of these diagnosed before surgical intervention. Many of the recommendations for dvt prophylaxis after foot and ankle surgery have been extrapolated from the total joint arthroplasty literature. (3) the time course for development of postoperative vte may differ with the type of surgery:
Deep venous thrombosis prophylaxis in surgical patients summary critically ill patients are at significant risk for deep venous thrombosis (dvt) as a result of inactivity, immobilization, vascular injury, and/or hypercoagulable states. Thromboprophylaxis is recommended, anticoagulant prophylaxis should start at least 12 hours after surgery (usually the morning after surgery). Of the 27 patients with dvt, 3 had a proximal dvt and 24 had a distal dvt.
Vte prophylaxis after major surgery. When in doubt about the risk of vte, a modified caprini risk assessment score can be used. The data supporting the use of lmwh was characterized as high.
Comprising deep vein thrombosis (dvt) and pulmonary embolism. In europe, traditionally, prophylaxis is started 12 hours before surgery, whereas in north america it is initiated 12 to 48 hours postoperatively.